
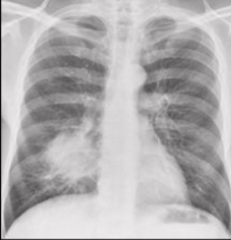

Right heart border is being blurred/lost


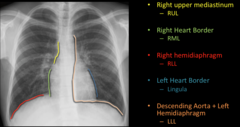
-Surrounding airspace if fluid filled
-More suggestive of pneumonia than atelectasis

-Nonsegmental
-Effects entire lobe
-Commonly caused by streptococcus pneumoniae and klebsiella
-usually heals without sequela

-Klebsiella classically, S. Pneumo more common
-“Bulging fissure”

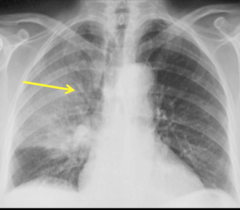
-Patchy nodular opacities
-S. Aureus, or G- organisms
-Scarring after healing
-Findings; bilateral medial lower low basal segment, right more common than left.
-Can become necrotic, capitate, and form an abscess.
-Any patient that cannot protect their airway is at risk.

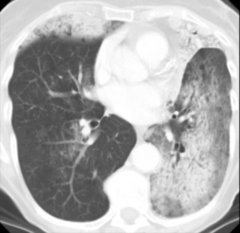
-Inflammation of interstitium
-Bilateral symmetric linear reticular opacities
-CT; Ground glass, whatever the &(%$ that is.
-Cancer
-Timeline differentiates them.
-Many known causes
-Findings; variable appearances with migratory multifocal peripheral opacities.
-Clinical; patient with protected nonproductive cough and low grade fever with restrictive pattern on PFT. Does not respond to antibiotics, does respond to steroids.
-Good prognosis.
-Halo border
Acutely present or subside on serial imaging

-Due to mixed anaerobic infection (S Aureus, pseudomonas)
-Often related to aspiration, poor dental hygiene, LOC, esophageal dysmotlity, neurological disease
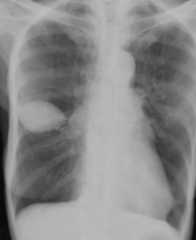
-Multiple peripheral basilar nodules, which may cavitate.
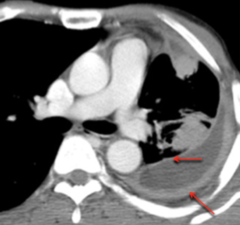
-Some may show a feeding vessel, and an infarct
-Related to IVDU, and bacterial tricuspid valve endocarditis
-Staph Aureus and epidermis.
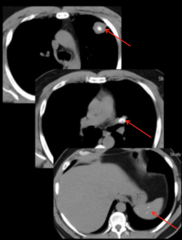
-Often related to evolution of a parapneumonic effusion, or an underlying lung infection that erupts into the pleural space (abscess or septic emboli).
-Often located
-Split Pleural sign
-Caused by infectious and non-infectious causes
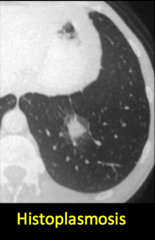
-Common infectious causes; Histo and TB.
-Often seen with calcified hilar/mediastinal lymph nodes and hepatic/splenic granulomata.
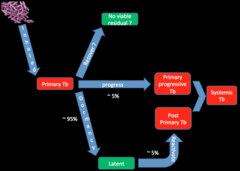
-Usually asymptomatic in children, only detected via PPD.
-Symptomatic in adults.
-FTT, night sweats, weight loss, hemoptysis.
-Often no imaging signs.

-Mediastinal and ipsilateral hilar lymphadenopathy in children and immunocompromised. Atelectasis may occur from compression of central airways.
-Plural effusion, usually small, isolated, and unilateral.
-Findings clear slowly.
-Ranke Complex; Calcified tuberculoma and ipsilateral hilar lymph node.
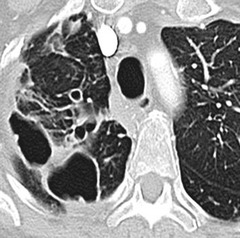
-Extensive consolidation and cavitation can develop.
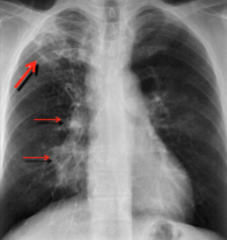
-Posterior upper lobe and superior segment of lower lobes is most common.
-Classically in the apical posterior upper lobes and superior segments of lower lobes.
-Rarely any pleural effusion or LAD.
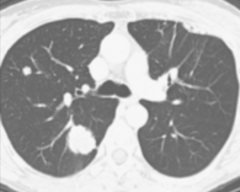
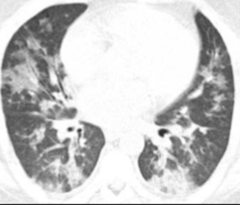
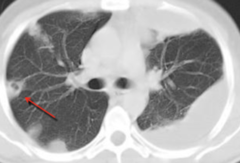
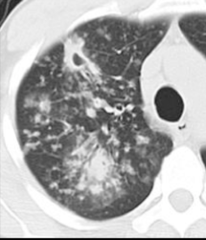
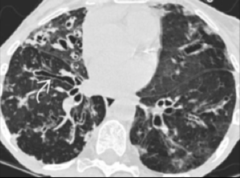
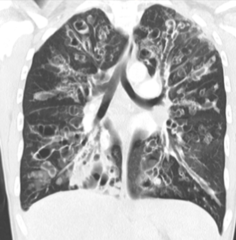
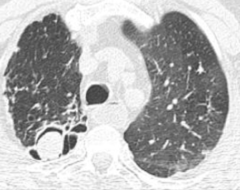
-May be associated with Tree in Bud opacities, which indicates the spread of the disease via the small airways. (Image)

-indicates hematogenous spread
-CD4<200; post primary resembles a primary infection; consolidation and LAD.
-Endobronchial spread
-Miliary Patterns
-Centrilobular nodules (tree in bud)
-Primary, progressive primary, post-primary.
-Linear scarring
-Calcified nodules.
-Stable for 6mos.
-From natural water, soil, and animals.
-Types; cavitary, bronchiectasis and nodules, centrilobular nodules.
-Symptom; chronic cough.
-Older men in 60s with COPD or mildly immunocompromised.

-Middle lobe and lingual predominant
-Women in their 60s.
-Lady Wndemere syndrome

-Owners of hot tubs
-“Hot tub lung”
-Bronchiectasis
-Upper lobe in central cystic/varicoid bronchiectasis
-Pseudomonas, aspergillus, mycobacterial infection
-Semi-invasive; mild immunocompromised patients. (Chronic necrotizing aspergillosis)
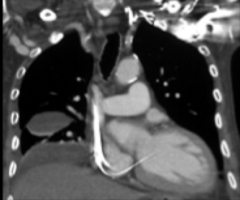
-Mycetoma; normal immunity, history of apical cavity.
-Findings; angio invasive (halos early, air crescent late), airway invasive (tree in bud and centrilobar nodules)
-Chronic necrotizing aspergillosis
-Findings like TB; upper lobe consolidation and cavity.
-Normal immunity
-History of apical cavity (prior TB, bull, abscess)
Fungus ball fills a preexisting cavity.




